Prevent Cancer Foundation responds to FDA approval of HPV self-collection screening
This week, the Food and Drug Administration (FDA) approved human papillomavirus (HPV) self-collection screening. Previously, HPV testing could be performed only by a health care provider, but now people will be able to collect their own samples in a private room at their provider’s office or other health care facility (similar to how you would collect your own urine sample, only this is with a vaginal swab).
The Prevent Cancer Foundation® is optimistic about increased access and a new option for early detection of HPV. Since this test can be done at urgent care clinics, doctors’ offices and pharmacies, it may eliminate some barriers to getting this vital screening. Those in medically underserved areas may no longer need to travel long distances to get screened, and those avoiding a screening due to discomfort with the procedure could now opt to collect their own sample for testing.
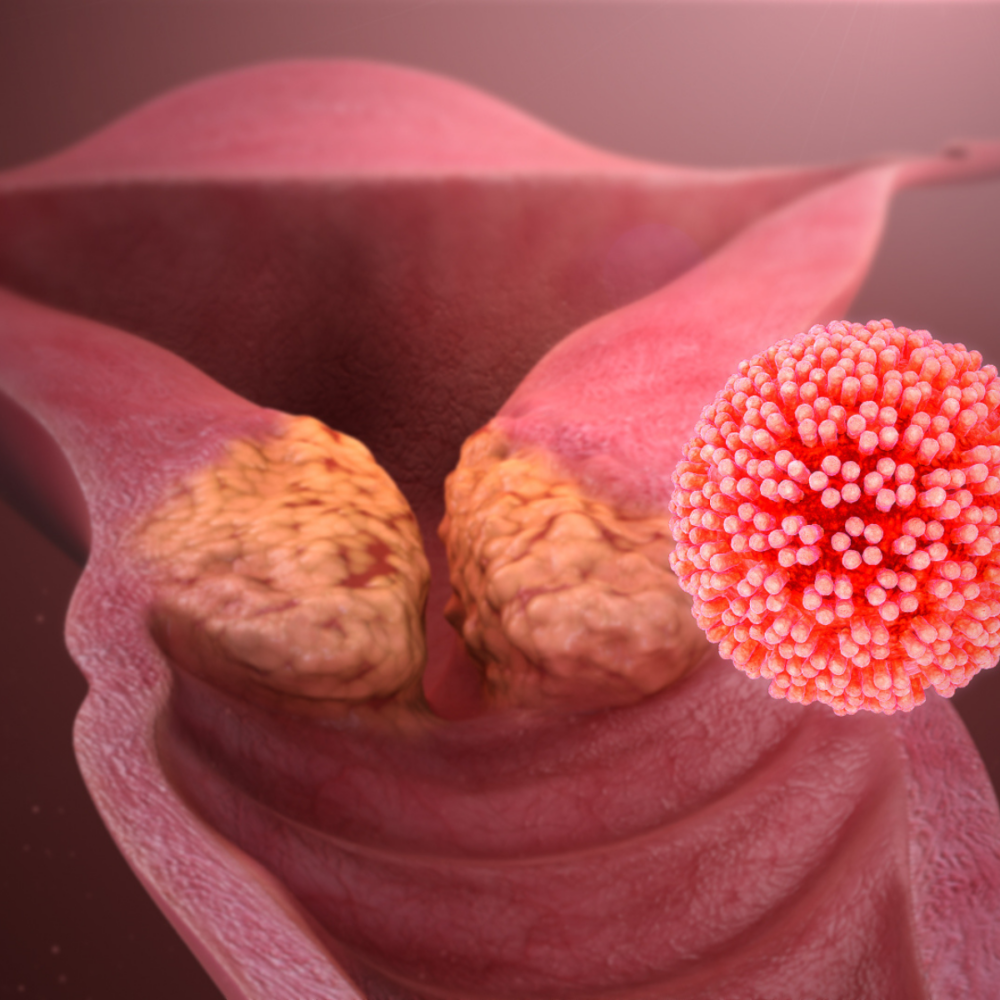
HPV screening is paramount to preventing cancer. The virus causes more than 90% of cervical cancer cases, but by detecting and treating HPV, you can stop cervical cancer before it starts. By increasing access to HPV testing, we can prevent more cancers and save lives.
HPV self-sampling in a health care setting is also the first step toward making at-home testing available, which would further increase access. In the Prevent Cancer Foundation’s 2024 Early Detection Survey, 26% of women who are behind on their routine cervical cancer screening said that they would prioritize their screening if an at-home test option were available—and 24% said they would prioritize it if there were a different or less invasive test or screening. This self-sampling indicates major progress in making those options a reality for women and people with a cervix in the U.S.
This screening option does not replace the need for your annual primary care and gynecologist visits, where other important health care conversations and checks take place.
To protect yourself from HPV and reduce your risk of cancer, you should get vaccinated against the virus. HPV vaccination is recommended for all young people beginning at age 9 and up to age 26. (If you are age 27-45, HPV vaccination is FDA-approved. Talk to your health care provider to see if it makes sense for you.)
HPV is also linked to at least five other types of cancer including vulvar, vaginal, penile and anal cancers, as well as oropharyngeal cancer, a cancer of the back of the throat, including the base of the tongue and tonsils.
In addition to HPV testing, Pap tests are available to screen for cervical cancer. With routine screening, you can find precancerous cervical cells (which can later be removed) before they become cancer or you can detect cancer early, which can lead to better outcomes.
If you are of average risk, follow these screening guidelines:
- Ages 21–29: Have a Pap test every 3 years.
- Ages 30–65: Have any of these options:
- A Pap test alone every 3 years.
- A high-risk HPV test alone every 5 years.
- A high-risk HPV test with a Pap test (co-testing) every 5 years.
If you are at increased risk for cervical cancer because of a suppressed immune system (for example, from HIV infection, organ or stem-cell transplant or long-term steroid use), because you were exposed to DES in utero or because you have had cervical cancer or certain precancerous conditions, you may need to be screened more often. Follow the recommendations of your health care provider.
After age 65, talk with your health care provider about whether you still need to be screened.