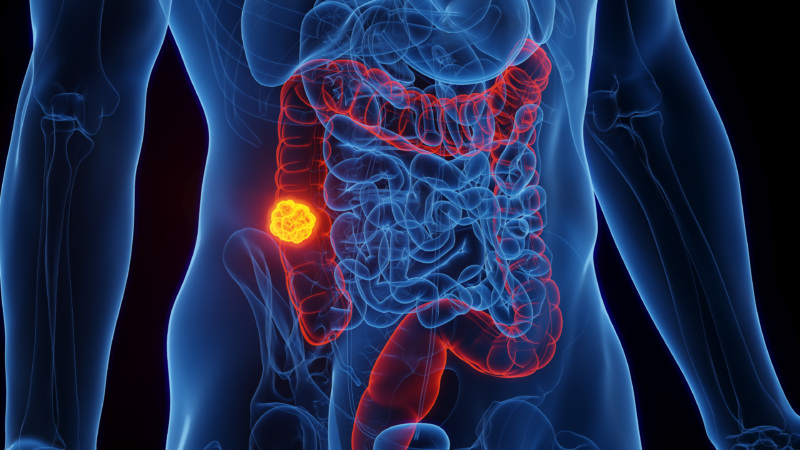
Ages 45–75: Get screened
Start getting screened at age 45 if you’re at average risk for colorectal cancer. See below for more on the screening options that may be available for you. Continue getting screened through age 75 if you are in good health with a life expectancy of 10 years or more.